“I feel I watched a miracle in progress” – Delia Burley
Delia Burley was a volunteer on the Council of Iain Rennie Hospice at Home when it was first established in 1985. She talks about the challenges the organisation faced, the joy of being involved, and the ‘miracle’ of watching it grow into the organisation it is today.
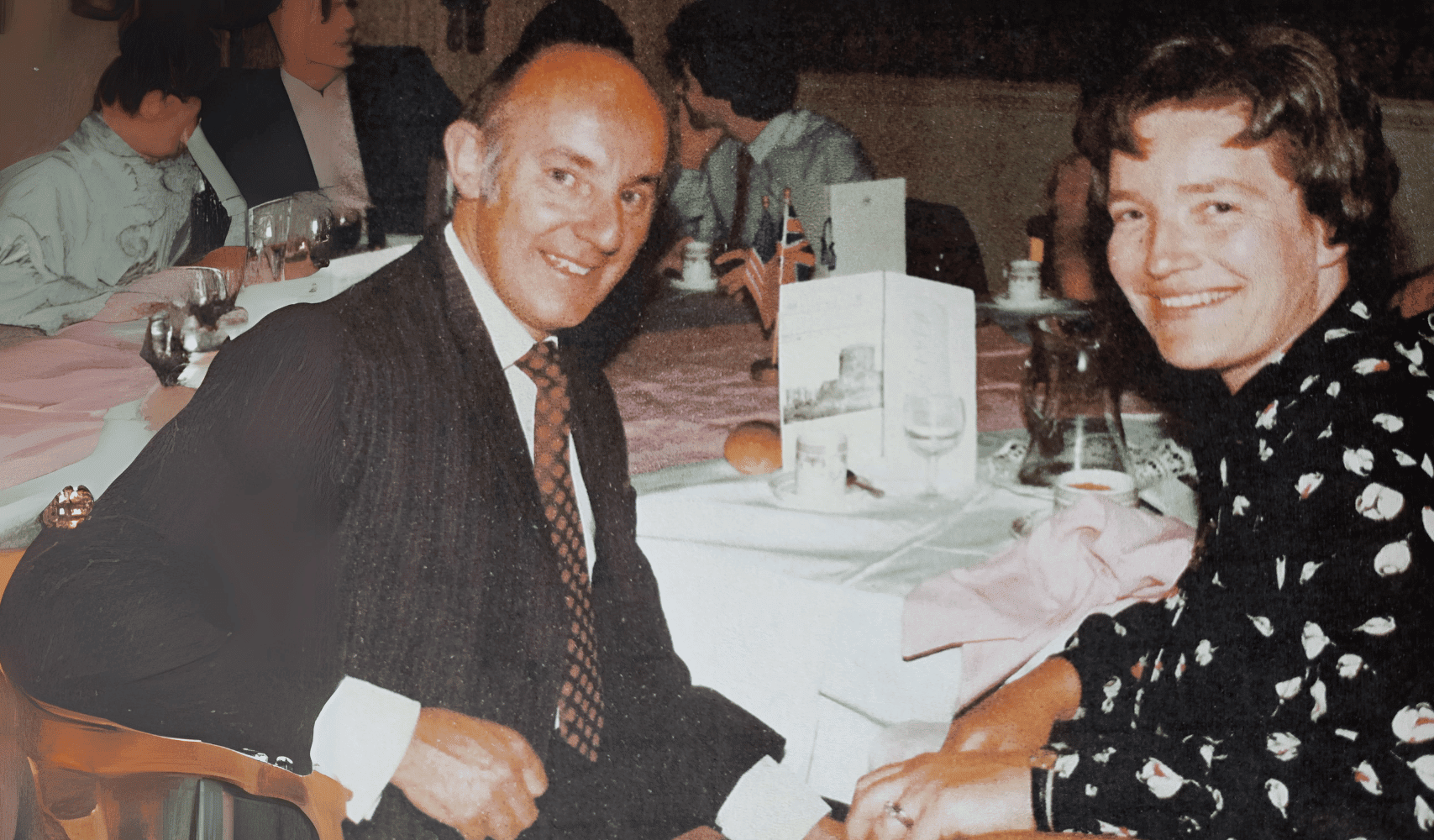
Delia says, “Cicely Saunders came to lecture about hospice care when I was a medical student and I remember being inspired by her as an individual and by the concept of hospice care as a whole. I qualified in 1975 and completed my GP training in 1978. In 1983 my husband and I moved to Beaconsfield with our two young children.
“That’s where I met Mary Robson who was one of the founding nurses of Iain Rennie Hospice at Home. In the summer of 1985 Mary’s husband, Eric, asked me if I would come to a meeting with a view to establishing a hospice at home. At the time I was working part time in the diabetic department of the local hospital as it fitted with family life. To find out more, I went along to Mary and Eric’s home and I was so impressed with their vision and the conviction of the nursing team.
“It was clear to me that providing end of life care for a person in their own home was the right thing to do, the best model of care.”
“My husband experienced ill health all his life and I have spent many days and nights beside him in hospital. It is an exhausting, worrying time, giving a sense of powerlessness. If you can care for an ill person at home, some elements of normal family life continue. This is of enormous benefit to patient and family alike.
“Shortly after the meeting in 1985, I became a volunteer on the Council of Iain Rennie Hospice at Home. I was involved in making sure the nurses were supported and getting the right training and education to provide the best care they could. The nurses would tell me where they felt they had a gap in expertise and I would arrange for a specialist to come and speak with them, such as a physiotherapist or cancer specialist. Although my husband, Chris, didn’t have an official role within the hospice, he advised on financial affairs informally.
“The nurses had such faith in what they were doing and used to say: ‘we will carry on nursing – the money will come’.”
“We were involved in fundraising too as we were completely dependent on people putting their hands in their pockets. In the first year, the hospice only had funds to pay the nurses for the next fortnight. The nurses had such faith in what they were doing and used to say: ‘we will carry on nursing – the money will come.’
The beauty of bringing hospice care into the home is that we didn’t need funding for a building or beds because everything was provided in people’s homes. Initially the council meetings were held at our home and everyone joked that the coffee pot was constantly brewing.
“It took several years for the local medical community to recognise us as an official organisation”
“Funding was just one of the many challenges we faced. Because our organisation was nurse-led and didn’t employ our own doctor, it took several years for the local medical community to recognise us as an official organisation. They considered our approach innovative and we had to prove ourselves.
“My husband died at home in 2022 after a long illness. He did not have significant pain so he did not need physical hospice at home care. The Rennie Grove Hospice nurses became involved at a managerial level; liaising with district nurses, organising the supply of equipment, and making sure that I personally, as a sole carer, was coping. They were very alert to my stress. Our family could still have an element of normal life, friends could visit and I could ‘escape’ into the garden for moments of peace. That all helped Chris to ‘live’ to the end, in a familiar environment, rather than just wait for the end to come in a hospital.
“The night Chris died I was at my most vulnerable. The Rennie Grove Hospice at Home team came out and they were brilliant, they helped me get through an exceptionally long and difficult night.
“It is a privilege to go into a person’s home at a time when they are most vulnerable.”
“My advice to anyone starting out in hospice at home care is to respect the sanctity of the patient’s home. It is a privilege to go into a person’s home at a time when they are most vulnerable. It’s also vital to listen to what an individual and family want. You need to listen more than you need to talk. It can be a very bewildering time for families and it’s important to be sensitive to their needs.
“I feel incredibly grateful to have been there at the beginning and to see the hospice grow. I feel I watched a miracle in progress.”